“Congenital” Trigger Thumb
Dr Stuart J.D. Myers
MB. B.S. Hons (NSW), F.R.A.C.S. (Orth)
www.myhand.com.au


Trigger finger, also called “Stenosing Tenosynovitis”, is a common hand ailment in adults. The first sign of the condition may be clicking when bending a finger to make a fist. Later one may need to use the other hand to straighten the finger. When the finger does move, one may feel a snap or click, as it suddenly gets "unstuck". This is the triggering that gives the condition its name.
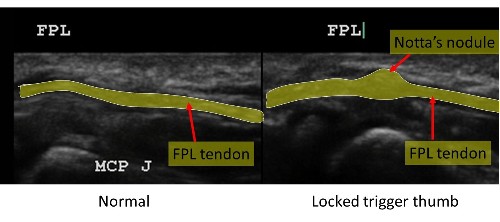
In adults a Trigger finger develops when the synovium around a tendon in a finger or thumb becomes chronically inflamed and / or thickened. The tendon starts catching as it enters the opening of the tunnel. The tendon bunches up on itself forming a nodule that can be felt in the palm.
The term “trigger” implies clicking of the thumb but most children present with a permanently bent or “flexed” thumb.
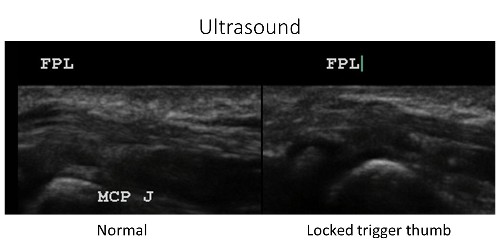
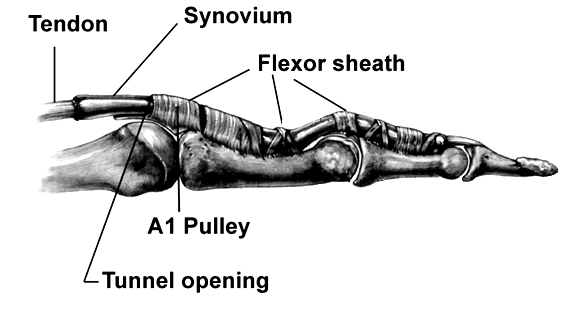
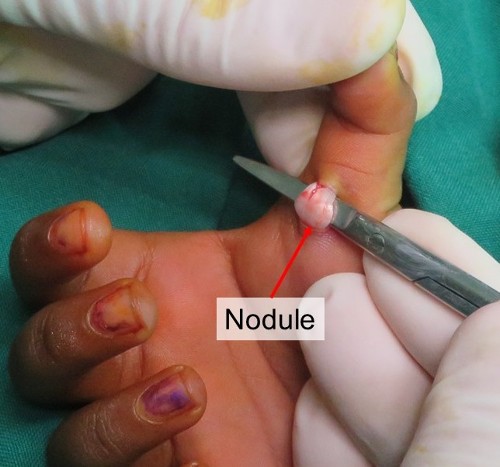
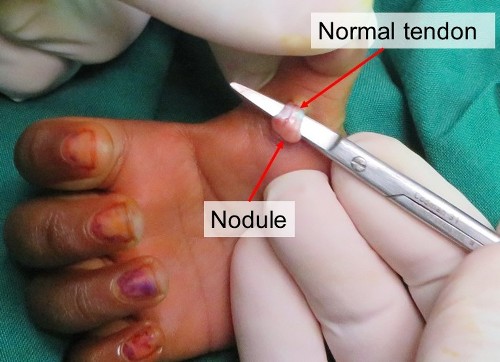
The cause is unknown. It is either due to a nodule or thickening of the flexor pollicis longus tendon or narrowing of the flexor sheath, or both.
The nodule of the flexor tendon can be felt moving on the front of the thumb when the end joint of the thumb is gently flexed and extended.
Trigger thumbs are 10 times more common than trigger fingers in children.
The incidence of trigger thumbs is about 3/1000. Both thumbs are involved in 25% cases.
The term “congenital” is probably also a misnomer because it is rarely if ever seen in newborns and must therefore develop later.
The diagnosis of a trigger finger is made with a simple physical examination.
X-rays and other tests generally are not needed unless multiple fingers are triggering. In this case blood tests are recommended to exclude an underlying cause for the triggering
eg Diabetes or an inflammatory arthritis.
The ultrasound below reveals the large nodule on the tendon but is not necessary to diagnose the condition.
Anatomy
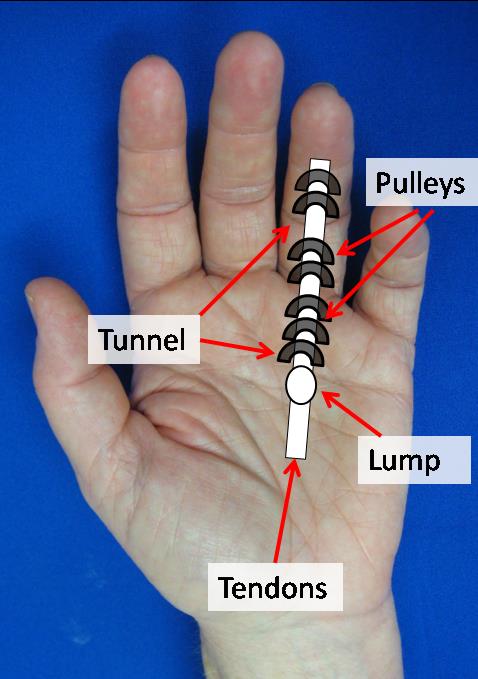
Along the palmar surface of each finger and thumb there is a smooth tunnel called the flexor sheath.
The tendons that bend the thumb run in this tunnel.
The normal thickenings of the tunnel are called pulleys and these prevent the tendons from bowstringing when the finger or thumb bends.
The tunnel is lined by synovium – a tissue which lubricates the tunnel.
Treatment
The Natural History is poorly understood. If the diagnosis is made before 12 months of age about 1/3 of cases will eventually resolve over a prolonged period of 5 yrs.
1. Night time splinting for an average of 6 - 12 months if flexible ( Uncommon) - 75% resolve.
2. Gentle thumb stretching ( uncommon)
3. Surgery – If thumb locked in flexion (common)
Surgery:
The timing of surgery depends on multiple factors;
- Age of the child,
- Pain and decreased use of thumb
- If deformity is fixed or flexible
- Patience of the family.
Delay in surgery if the child is less than 3 years of age is not a disaster. It does not result in permanent thumb stiffness or tendon damage.
Children with painful triggering and a fixed flexion deformity > 12 months old should have surgery.
Surgical Technique


Few hours in Hospital ( Day only)
General Anaesthetic
Small incision on front of thumb
Identify and retract the nerves and arteries
Release the A1 pulley
Leave the nodule – it will decrease over time
The thumb is extended fully
Wound sutured with 60 Vicryl Rapide - an absorbable suture.
Bandage for 1 week – Keep dry. Plastic bag over hand when showering
The dressings are removed at 1 week and the wound is washed in soapy water
Cover the wound with a bandaid until the sutures fall out
Use the thumb as pain permits
Therapy is not generally necessary.
Outcome
Surgery will reliably relieve the problem. Most children have returned to full activity in 3 - 4 weeks.
Recurrence is extremely rare
Complications are rare.
- Thick or tenderness in the scar
- Tendon bowstringing
- Altered sensation
16 February 2020
