Complex regional pain syndrome (C.R.P.S.) was previously referred to as REFLEX SYMPATHETIC DYSTROPHY (RSD).
It is a condition characterised by 5 main features:
1. Severe Pain
2. Swelling
3. Stiffness
4. Skin discolouration
5. Abnormal sweating or dry skin
Normal C.R.P.S. Normal C.R.P.S.


Other possible features include:
6. Tremor
7. Altered sensation
8. Shoulder pain and stiffness
9. Depression
10. Osteoporosis noted on Xray
11. Bone scan abnormalities with diffuse increased uptake around the joints.
Normal Osteoporosis in C.R.P.S.
Normally pain is a warning signal that the body is at risk of injury or damage.
The pain in a CRPS is disproportionate to the injury or stimulus applied.
This does not mean that it is not real. It may extend to effect the whole arm or leg.
The pain may be of a “burning “ quality and is described as “Neuropathic” or nerve generated pain. Pain in a CRPS is not associated with tissue damage.
![]()
If one experiences Pain > 6/10 where 10 is the most severe pain imaginable more than 48 hours after an injury then something is wrong. The commonest causes are: - Plaster cast too tight, Nerve compression or an early CRPS.
CAUSE:
The cause is poorly understood, although Psychological, Physical & Environmental factors play a role in its development.
There may be genetic factors that predispose an individual to this condition.
It is believed that there is a chemical change at the spinal cord level, which “sensitises” the pain receptors. When the pain receptors are sensitised even light touch on the skin can become a painful stimulus ( this is referred to as "Allodynia").
In a normal situation the brain has the ability to dampen down ones perception of pain. This occurs by signals travelling down from the brain to provide an inhibiting effect (-ve influence) on the pain receptors in the spinal cord. In this way a footballer may keep playing with a broken arm because his mind is so focused on the game. Once the game is over he may then realise that the arm is broken & he begins to perceive the pain. The brain also has the ability to increase our perception of pain by causing a +ve effect at the spinal cord. In this way it is believed that people who are very anxious or depressed have a greater perception of pain.
In a CRPS the +ve effect at the spinal cord level may be very prolonged or even permanent. This does not imply that you are "dreaming up the pain". The pain is very real and there are definite chemical changes at the spinal cord level.
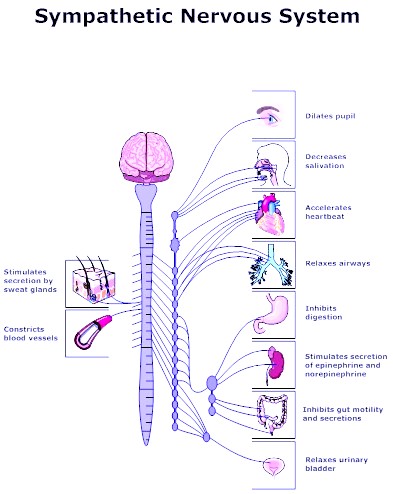
A secondary effect of a CRPS may result in abnormal firing of the sympathetic nerves. The sympathetic nerves are not normal nerves for feeling sensation or for causing muscles to contract. Rather, the sympathetic nervous system is used for controlling the heart rate, causing hairs to stand on end and causing sweating and colour changes in the skin. The sympathetic nerves are “automatic” nerves over which we have little direct control.
A CRPS may be triggered by a variety of causes such as minor trauma or even surgery. It not infrequently follows trauma to nerves. It appears to occur more frequently in patients who are anxious or depressed although this is certainly not always the case. There may be a genetic predisposition to this condition, which may run in families.
TREATMENT:
Treatment is best in a multidisciplanary pain clinic setting involving
- Anaesthetists (Pain clinic Specialists). Dr Jordon Wood - Prince of Wales Pain Clinic
- Psychologists
- Physiotherapists
1. Drugs:
The aim is to break the pain cycle & control the inflammation. It involves aggressive early management of the pain. Often normal painkillers are not effective.
Neuropathic pain medications appear to have a specific effect at dampening down nerve irritability.
e.g. Lyrica, Tryptanol. Gabapentin - The biggest side effect is drowsiness so we start with a low dose.
Review the “Product Information” on these drugs to be aware of potential side effects.
Anti-inflammatory drugs e.g. Voltaren may also be used.
2. Sympathetic Blocks: It may also involve sympathetic blocks, which involve injections either around the nerves in the neck, or arm or injections into the veins. This is done as a day procedure in the pain clinic by an anaesthetist who is highly skilled in the treatment of this condition.
3. Local anaesthetic creams may be used. Local anaesthetic injections may also be used around nerves to block the pain and also as a test.
4. Hand Therapy:
The treatment also involves intensive hand therapy, which may involve encouragement of use of the injured limb.
- (a) Control swelling – Isotoner gloves
- (b) Exercise programme
- (c) “Mirror Box Therapy”
- This is an evidence based programme created by the Neuro Orthopaedic Institute ( NOI Group)
- Aimed at overcoming the brains tendency to “ignore” the injured limb.
- If you put your left hand behind a mirror and right hand in front, you can trick your brain into believing that the reflection of your right hand in the mirror is your left. You are now exercising your left hand in the brain, particularly if you start to move your right hand.
More information Motor Imagery http://www.gradedmotorimagery.com/index.html.
Download an Exercise App. http://www.noigroup.com/en/Product/BTRAPP
Search "Recognise" in the App store ~ $10
- (d). T.E.N.S. (TRANSCUTANEOUS ELECTRICAL NERVE STIMULATION) : Other physiotherapy modalities include a TENS machine which involve a minor electrical stimulation of the hand or arm to reduce the amount of pain.
5. Positive Outlook This is a very frustrating condition. There is no doubt that a positive approach will help the situation. In general pain is a warning. In this condition pain is a nuisance but does not equal damage - so you should endeavour to continue to do as much as you can, knowing that you are not causing damage to the effected arm or leg by using it.
6. More Information
- Manage Your Pain, 3rd Edition by Michael Nicholas et al – Book on pain management
- ACI Pain Management Network - Very useful NSW Government website on chronic pain.
PROGNOSIS:
The condition may take months to years settle down.
- 75% of patients improve dramatically with time returning to normal or very near normal.
- 15% of patients have moderate permanent disability &
- 10% of patients have severe permanent disability.
A rough guide is that a CRPS will triple the time it takes to recover from a given injury.
Revised 21 / 6 / 2015